On top of that, you have to require "knowledgeable care." This implies a physician should get the treatment as well as the treatment have to be provided daily by a signed up nurse, physiotherapist, or accredited functional nurse. Ultimately, Medicare only covers "acute" treatment as opposed to custodial care. This suggests it covers care only for people who are likely to recuperate from their problems, not care for people who require ongoing aid with carrying out daily activities, such as bathing or dressing. Contact your State Health Insurance Policy Help Program for free therapy solutions if you need assistance submitting a grievance versus your knowledgeable nursing facility. The Medi-Cal program spends for a substantial portion of psychological wellness therapy in The golden state.
Is rehab covered by Medicare?

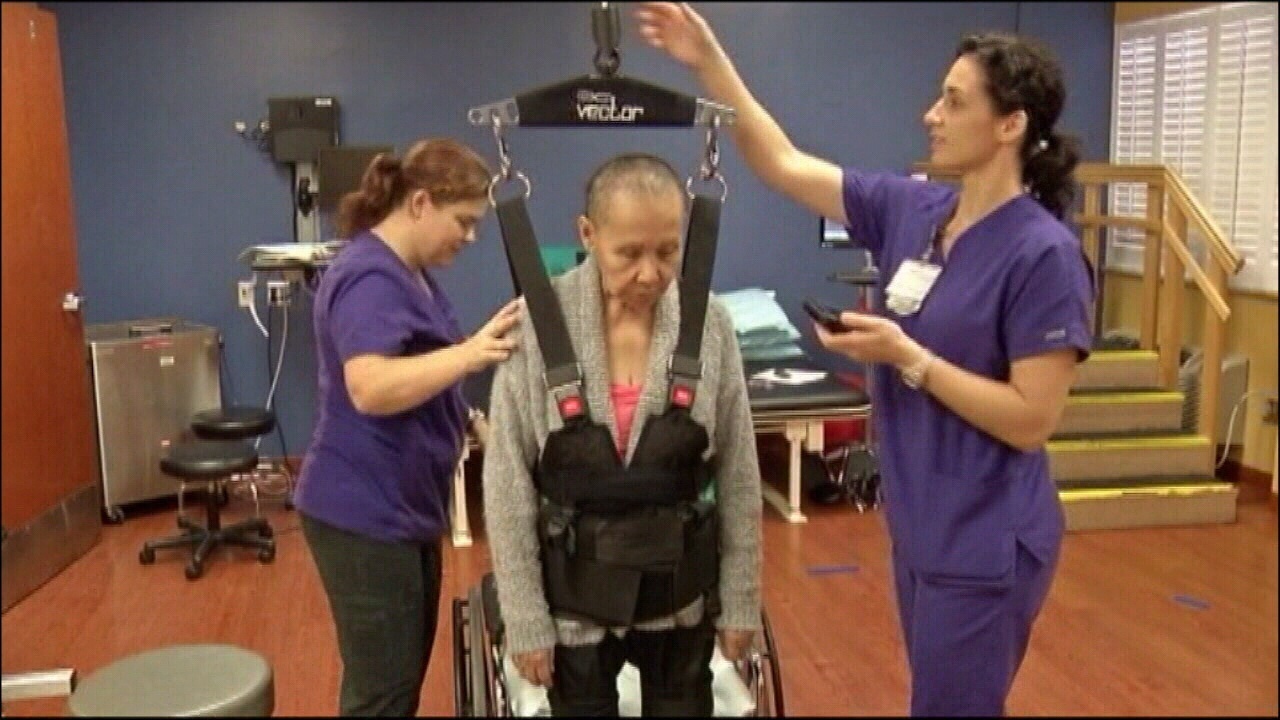
Medicare Part A covers care in a hospital rehab unit. Medicare Alcohol Abuse Treatment may pay for rehab in a skilled nursing facility in some cases. After you have been in a hospital for at least 3 days, Medicare will pay for inpatient rehab for up to 100 days in a benefit period. A benefit period starts when you go into the hospital.
Unlike regular business insurance policy, Medicare can pay either the client or the provider, depending on the job. If your company has actually accepted job by Medicare, it implies that he or she has accepted accept the Medicare permitted quantity as complete settlement on Medicare cases. A vital point to comprehend about Medicare Part B invoicing is that everyone should pay a costs each month, and also pay an annual deductible and also copay. Thus, Part B is a whole lot like regular commercial insurance strategies.
What happens when you run out of Medicare days?
Medicare will stop paying for your inpatient-related hospital costs (such as room and board) if you run out of days during your benefit period. To be eligible for a new benefit period, and additional days of inpatient coverage, you must remain out of the hospital or SNF Addiction Treatment for 60 days in a row.
Mental wellness services may include treatment for depression, actions, or anxiety illness. Your medical professional can give you with some outpatient mental wellness services. Behavior health services such as psychotherapy as well as medication monitoring are offered to L.A
Differences In Coverage.
- . It needs to be offered by, or under the guidance of, proficient nursing or therapy staff.
- The house health and wellness agency should give you a notice called the Breakthrough Recipient Notice" (ABN) prior to giving you solutions as well as products that Medicare doesn't cover.
- A QIO is a group of doctors as well as various other experts that monitor the quality of treatment delivered to Medicare recipients.
- Sign up for get e-mail (or message) updates with crucial due date suggestions, valuable ideas, as well as various other info regarding your medical insurance.
- The person, in this situation, is accountable for paying the whole claim off to the carrier.
- Health And Wellness Resources as well as Solutions Administration centers, where you pay what you can pay for.
So, if somebody is discharged from the medical facility to a skilled nursing facility that is also an assisted living home, the person may not need to alter facilities as soon as their knowledgeable nursing needs are full. If that client is eligible for Medicaid, and also the assisted living facility is additionally a Medicaid-certified, they may continue to stay in the house under the Medicaid benefit.
Register for get email (or message) updates with important due date suggestions, valuable pointers, and also other information regarding your medical insurance. Out-of-pocket maximum This is the https://calendar.google.com total amount you'll have to pay regardless of just how much covered care you get in a strategy year. Having health protection can help protect you from high, unanticipated prices like these. See if you qualify for a Special Enrollment Duration 2020 Open Enrollment mores than, but you may still be able to register in 2020 medical insurance with a Special Registration Period. You should be under the treatment of a physician, and also you should be obtaining services under a plan of treatment created as well as reviewed routinely by a medical professional.
How can I get my insurance to pay for therapy?
If you have insurance benefits that include mental health coverage you may use those insurance benefits to seek treatment. Alternately, all Albertans have mental health coverage through Alberta Health Services. To access this coverage you can call Health Link (811) and ask for a referral to a mental health specialist.
PASC-SEIU Plan
This includes used habits evaluation and similar evidence-based treatments. The solutions should create, boost, or recover, as high as possible, the daily performance of a member with ASD. You will need previous authorization from your health insurance prior to you or a relative obtains domestic care therapy. You can file an issue with your health and wellness plan if your plan states the therapy is not clinically necessary. Psycho therapist - A licensed professional that gives scientific treatment or counseling for a selection of mental health care conditions.
Does medical pay for mental health services?
For low-income seniors, Medi-Cal also covers services not paid for by Medicare, including nursing home care. The Medi-Cal program pays for a significant portion of mental health treatment in California. County operation of Drug Medi-Cal and the Drug Medi-Cal Organized Delivery System.